Cholera Management in Iraq: Challenges, Strategies, and the Path Forward
DOI:
https://doi.org/10.59675/V223Abstract
The article discusses the ongoing challenges and management of cholera, particularly in Iraq, which is experiencing a resurgence of the disease. The bacteria Vibrio cholerae is the cause of cholera, which is mainly transmitted via tainted food and water. If left untreated, cholera can be fatal and cause severe dehydration. The article highlights the historical context of cholera outbreaks, the factors contributing to its prevalence in impoverished nations, and the specific situation in Iraq, where inadequate sanitation, malnutrition, and the aftermath of conflict exacerbate the problem.Efforts to manage cholera include rapid intervention, infection control, and public awareness campaigns. Organizations like WHO and UNICEF provide resources for cholera management, emphasizing the importance of early detection and treatment. The article also outlines the epidemiology of cholera, noting its endemic presence in various regions and the impact of climate change on outbreaks. Challenges to cholera prevention include poor healthcare infrastructure, political instability, and environmental factors. The article advocates for improved water and sanitation services (WASH), vaccination campaigns, and better healthcare facilities to reduce cholera incidence. It concludes that sustained efforts and funding are necessary to combat cholera effectively and improve health outcomes in affected regions.
References
Nayyar, A. and Privor-Dumm, L., 2020. Cholera control and prevention: Role of evidence-based advocacy and communications. Vaccine, 38, pp. A178-A180.
Chowdhury, F., Ross, A.G., Islam, M.T., McMillan, N.A. and Qadri, F., 2022. Diagnosis, management, and future control of cholera. Clinical Microbiology Reviews, 35(3), pp.e00211-21.
Qamar, K., Malik, U.U., Yousuf, J., Essar, M.Y., Muzzamil, M., Hashim, H.T. and Shah, J., 2022. Rise of cholera in Iraq: A rising concern. Annals of Medicine and Surgery, 81, p.104355.
S. Kanungo, A.S. Azman, T. Ramamurthy, J. Deen, S. Dutta, Cholera [Internet] The Lancet, 399, Elsevier B.V., 2022 [cited 2022 Jul 2]. p. 1429–40. Available from: htt ps://pubmed.ncbi.nlm.nih.gov/35397865/.
Cho, Y.J., Yi, H., Lee, J.H., Kim, D.W. and Chun, J., 2010. Genomic evolution of Vibrio cholerae. Current opinion in microbiology, 13(5), pp.646-651.
Rahmawaty, A., 2023. The Development of Cholera Vaccine Production: A Literature Review. Lux Mensana: Journal of Scientific Health, pp.115-125.
Al-Obaidi, R.M., Arif, S.K., Abed, R.M., Yaaqoob, L.A., Mahmood, S.A.F., Mohammed, S.J.A. and Abdulrahman, N.M., 2023. Vibrio cholerae: epidemiology, surveillance and occurrence in iraq. One Health Triad, Unique Scientific Publishers, Faisalabad, Pakistan, 2, pp.80-86.
Poulos C, Riewpaiboon A, Stewart JF, Clemens J, Guh S, Agtini M, et al. Costs of illness due to endemic cholera. Epidemiol Infect 2012;140(3):500–9.
Sarker AR, Islam Z, Khan IA, Saha A, Chowdhury F, Khan AI, et al. Cost of illness for cholera in a high risk urban area in Bangladesh: an analysis from household perspective. BMC Infect Dis 2013;13:518.
WHO fact sheet on cholera. Last up-date October 2016 http://www.who.int/mediacentre/factsheets/fs107/en/.
Thacker, S. B., & Berkelman, R. L. (1988). Public health surveillance in the United States. Epidemiologic Reviews, 10, 164-190.
[3] World Health Organization. Cholera resources can be found at http://www. who.int/cholera/en/ [Accessed 1/10/2017].
UNICEF Cholera Toolkit http://www.unicef.org/cholera_toolkit/ especially Chapter 8: Case management and infection control in health facilities and treatment sites pp110-135 [Accessed 1/10/2017].
MSF Cholera Guidelines http://www.humanitarianlibrary.org/resource/msfcholera-guidelines-0 [Accessed 1/10/2017]. [6] Stop Cholera https://www.stopcholera.org/ has a large number of fact sheets and toolkits [Accessed 1/10/2107].
Pietroni MAC. Cholera, Method of in Conn’s Current Therapy, Bope ET, Kellerman RD. editors. Philadelphia: Elsevier; 2017. p. 497–500. [8] Harris JB, Pietroni MAC. Approach to the child with acute diarrhea in resource limited countries. In: Calderwood SB, Bloom A, editors. UpToDate. Waltham, MA: UpToDate; 2017.
LaRocque R, Pietroni MAC. Approach to the adult with acute diarrhea in resource limited countries. In: Calderwood SB, Bloom A, editors. UpToDate. Waltham, MA: UpToDate; 2017
Deen J, Mengel MA, Clemens JD. 2020. Epidemiology of cholera. Vaccine 38:A31–A40. Crossref. PubMed. Web of Science.
Goel AK, Jiang SC. 2010. Genetic determinants of virulence, antibiogram and altered biotype among the Vibrio cholerae O1 isolates from different cholera outbreaks in India. Infect Genet Evol 10:814–818. Crossref. Web of Science.
World Health Organization. 2010. Cholera vaccines: WHO position paper—March 2010. Wkly Epidemiol Rec 85:117–128. PubMed.
World Health Organization. 2017. Cholera, 2016. Wkly Epidemiol Rec 92:521–536. PubMed.
Deen J, Mengel MA, Clemens JD. 2020. Epidemiology of cholera. Vaccine 38:A31–A40. Crossref. PubMed. Web of Science.
Harris JB, LaRocque RC, Qadri F, Ryan ET, Calderwood SB. 2012. Cholera. Lancet 379:2466–2476. Crossref. PubMed. Web of Science.
Mandal S, Mandal MD, Pal NK. 2011. Cholera: a great global concern. Asian Pac J Trop Med 4:573–580. Crossref. PubMed. Web of Science.
O’Connor KA, Cartwright E, Loharikar A, Routh J, Gaines J, Fouché M-DB, Jean-Louis R, Ayers T, Johnson D, Tappero JW, Roels TH, Archer WR, Dahourou GA, Mintz E, Quick R, Mahon BE. 2011. Risk factors early in the 2010 cholera epidemic, Haiti. Emerg Infect Dis 17:2136–2138. Crossref. PubMed. Web of Science.
Glass RI, Holmgren J, Haley CE, Khan MR, Svennerholm AM, Stoll BJ, Belayet Hossain KM, Black RE, Yunus M, Barua D. 1985. Predisposition for cholera of individuals with O blood group. Possible evolutionary significance. Am J Epidemiol 121:791–796. Crossref. PubMed. Web of Science.
Harris JB, Khan AI, LaRocque RC, Dorer DJ, Chowdhury F, Faruque ASG, Sack DA, Ryan ET, Qadri F, Calderwood SB. 2005. Blood group, immunity, and risk of infection with Vibrio cholerae in an area of endemicity. Infect Immun 73:7422–7427. Crossref. PubMed. Web of Science.
Larocque RC, Sabeti P, Duggal P, Chowdhury F, Khan AI, Lebrun LM, Harris JB, Ryan ET, Qadri F, Calderwood SB. 2009. A variant in long palate, lung and nasal epithelium clone 1 is associated with cholera in a Bangladeshi population. Genes Immun 10:267–272. Crossref. PubMed. Web of Science.
Karlsson EK, Harris JB, Tabrizi S, Rahman A, Shlyakhter I, Patterson N, O’Dushlaine C, Schaffner SF, Gupta S, Chowdhury F, Sheikh A, Shin OS, Ellis C, Becker CE, Stuart LM, Calderwood SB, Ryan ET, Qadri F, Sabeti PC, Larocque RC. 2013. Natural selection in a Bangladeshi population from the cholera-endemic Ganges River Delta. Sci Transl Med 5:192ra86. Crossref. PubMed.
Bavishi C, Dupont HL. 2011. Systematic review: the use of proton pump inhibitors and increased susceptibility to enteric infection. Aliment Pharmacol Ther 34:1269–1281. Crossref. PubMed. Web of Science.
Nsagha DS, Atashili J, Fon PN, Tanue EA, Ayima CW, Kibu OD. 2015. Assessing the risk factors of cholera epidemic in the Buea Health District of Cameroon. BMC Public Health 15:1128. Crossref. PubMed. Web of Science.
Sharifi-Mood B, Metanat M. 2014. Diagnosis, clinical management, prevention, and control of cholera; a review study. Int J Infect 1:e18303. Crossref.
Harris JB, LaRocque RC, Qadri F, Ryan ET, Calderwood SB. 2012. Cholera. Lancet 379:2466–2476. Crossref. PubMed. Web of Science.
Leung DT, Chowdhury F, Calderwood SB, Qadri F, Ryan ET. 2012. Immune responses to cholera in children. Expert Rev Anti Infect Ther 10:435–444. Crossref. PubMed. Web of Science.
Sauvageot D, Njanpop-Lafourcade BM, Akilimali L, et al. Cholera incidence and mortality in Sub-Saharan African sites during multi-country surveillance. PLoS NeglTrop Dis 2016;10(5):e0004679.
Guillaume Y, Ternier R, Vissieres K, Casseus A, Chery MJ, Ivers LC. Responding to cholera in Haiti: implications for the national plan to eliminate cholera by 2022. J Infect Dis 2018;218(suppl_3):S167–70.
Buliva, E., Elnossery, S., Okwarah, P., Tayyab, M., Brennan, R. and Abubakar, A., 2023. Cholera prevention, control strategies, challenges and World Health Organization initiatives in the Eastern Mediterranean Region: A narrative review. Heliyon, 9(5).
Camacho, M. Bouhenia, R. Alyusfi, A. Alkohlani, M.A.M. Naji, X. de Radigu`es, A.M. Abubakar, A. Almoalmi, C. Seguin, M.J. Sagrado, M. Poncin, M. McRae, M. Musoke, A. Rakesh, K. Porten, C. Haskew, K.E. Atkins, R.M. Eggo, A.S. Azman, F.J. Luquero, Cholera epidemic in Yemen, 2016-18: an analysis of surveillance data, Lancet Global Health 6 (6) (2018) e680–e690, https://doi.org/10.1016/S2214-109X(18)30230-4.
OCHA, Global Humanitarian Overview 2021, United Nations, 2021, https://doi.org/10.18356/9789214030751. [42] GTFCC, Statement from the Steering Committee of the Global Task Force on Cholera Control (GTFCC), 2022. https://www.tandfonline.com/doi/full/10.1080/ 21645515.2018.1504155.
WHO, Cholera situation in Yemen, Retrieved April 11, 2022. from, https://applications.emro.who.int/docs/WHOEMCSR314E-eng.pdf?
WHO, Cholera – Global Situation. Disease Outbreak News, December 16, 2022, https://www.who.int/emergencies/disease-outbreak-news/item/2022- DON426
Atwoli, G.E. Erhabor, A.A. Gbakima, A. Haileamlak, J.-M.K. Ntumba, J. Kigera, L. Laybourn-Langton, R. Mash, J. Muhia, F.M. Mulaudzi, D. Ofori-Adjei, F. Okonofua, A. Rashidian, M. El-Adawy, S. Sidib´e, A. Snouber, J. Tumwine, M.S. Yassien, P. Yonga, C. Zielinski, COP27 climate change conference: urgent action needed for Africa and the world, Lancet Public Health 7 (11) (2022) e892–e894, https://doi.org/10.1016/S2468-2667(22)00261-4.
Ngereza, C. and Mkomagi, J., 2022. Spatial Clustering of Cholera Deaths in Mainland Tanzania.
Deen, J., Mengel, M.A. and Clemens, J.D., 2020. Epidemiology of cholera. Vaccine, 38, pp.A31-A40.
D. Cutler, G. Miller, The role of public health improvements in health advances: the twentieth-century United States, Demography 42 (1) (2005) 1–22, https:// doi.org/10.1353/dem.2005.0002.
S. Moore, N. Thomson, A. Mutreja, R. Piarroux, Widespread epidemic cholera caused by a restricted subset of Vibrio cholerae clones, Clin. Microbiol. Infection: Off. Pub. Eur. Soci. Clin. Microb. Inf. Dis. 20 (5) (2014) 373–379, https://doi.org/10.1111/1469-0691.12610
WHO, Cholera outbreak in Sudan, Week. Epid. Mon. 12 (38) (2019). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_38.pdf?
WHO, Upsurge of cholera cases in Yemen, Week. Epid. Mon. 12 (12) (2019). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_12_12.pdf?
2] WHO, Oral cholera vaccine (OCV) campaign in Yemen, Week. Epid. Mon. 12 (21) (2019). https://applications.emro.who.int/docs/epi/2019/Epi_Monitor_2019_
T.R. Zolnikov, The maladies of water and war: addressing poor water quality in Iraq, Am J Public Health 103 (6) (2013 Jun) 980–987, 2013/04/18.
P.H. Gleick, Water as a weapon and casualty of armed conflict: a review of recent water-related violence in Iraq, Syria, and Yemen, WIREs Water 6 (4) (2019 Jul), e1351.
Iraq’s healthcare system is in crisis. Patients are suffering. [Internet]. [cited 2022 Jul 14]. Available from: https://www.reuters.com/investigates/special-report/ira q-health/
Cholera continues to spread in Iraq, UN health agency reports | | UN News [Internet]. [cited 2022 Jul 14]. Available from: https://news.un.org/en/story/ 2007/10/234872-cholera-continues-spread-iraq-un-health-agency-reports.
Iraq, Health services struggle to prevent cholera spreading - Iraq | ReliefWeb [Internet]. [cited 2022 Jul 14]. Available from: https://reliefweb.int/report/iraq/i raq-health-services-struggle-prevent-cholera-spreading.
Cholera [Internet]. [cited 2022 Jul 3]. Available from: https://www.who.int/ news-room/fact-sheets/detail/cholera.
WHO Provides Sulaymaniyah with urgent medical supplies to prepare for and respond to the recent Cholera outbreak | United Nations in Iraq [Internet]. [cited 2022 Jul 3]. Available from: https://iraq.un.org/en/186938-who-provides-sula ymaniyah-urgent-medical-supplies-prepare-and-respond-recent-cholera
The Ministry of Health,Iraq in cooperation with the World Health Organization, implements a training workshop for capacity building on risks [Internet] [cited 2022 Jul 3]. Available from: https://moh.gov.iq/?page=4124, 2022
sterilization tablets in unserved areas of the liquefaction network in Suq AlShuyoukh district]. Arabic [Internet] [cited 2022 Jul 3]. Available from: https:// moh.gov.iq/?page=4072, 2022
For the second day in a row, Karbala Health is carrying out a series of control tours in markets and shops throughout the governorate]. Arabic [Internet [cited 2022 Jul 3]. Available from: https://moh.gov.iq/?page=4140, 2022.
O.C.H.A. Iraq, Humanitarian bulletin - overview on humanitarian transition, May - June 2022 - Iraq ReliefWeb [Internet]. 2022 [cited 2022 Jul 2]. Available from: https://reliefweb.int/report/iraq/iraq-humanitarian-bulletin-overview-humanitar ian-transition-may-june-2022
O.C.H.A. Iraq, Humanitarian response plan 2022 - executive summary [EN/AR/ KU] - Iraq | ReliefWeb [Internet]. 2022 [cited 2022 Jul 2]. Available from: https: //reliefweb.int/report/iraq/iraq-humanitarian-response-plan-2022-executive-su mmary-enarku.
U.N.H.C.R. Opening, of new primary health care centre in Kawergosk to support the local and refugee communities [EN/AR/KU] - Iraq | ReliefWeb [Internet]. 2022 [cited 2022 Jul 2]. Available from: https://reliefweb.int/report/iraq/opening-ne w-primary-health-care-centre-kawergosk-support-local-and-refugee-communitie s-enarku.
Un-Habitat, UN-Habitat Iraq receives generous support from Korea International Cooperation Agency (KOICA) to promote peace and stability by facilitating sustainable returns [EN/AR] - Iraq | ReliefWeb [Internet] [cited 2022 Jul 2]. Available from: https://reliefweb.int/report/iraq/un-habitat-iraq-receives-genero us-support-korea-international-cooperation-agency-koica-promote-peace-and-stab ility-facilitating-sustainable-returns-enar, 2022.
UNDP, Norway reaffirms its commitment to stabilization in Iraq with US$ 7.5 million contribution [EN/AR] - Iraq | ReliefWeb [Internet [cited 2022 Jul 2]. Available from: https://reliefweb.int/report/iraq/norway-reaffirms-its-commi tment-stabilization-iraq-us-75-million-contribution-enar, 2022.
W.H.O. Unct Iraq, WHO marks five years of strategic partnership with USAID in Iraq - Iraq | ReliefWeb [Internet] [cited 2022 Jul 2]. Available from: https://relie fweb.int/report/iraq/who-marks-five-years-strategic-partnership-usaid-iraq, 2022.
Cholera in Iraq 2012 - Iraq | ReliefWeb [Internet]. [cited 2022 Jul 5]. Available from: https://reliefweb.int/report/iraq/cholera-iraq-2012.
WHO EMRO | WHO continues to support the cholera outbreak response in Iraq as cases decline | News | Epidemic and pandemic diseases [Internet]. [cited 2022 Jul 5]. Available from: http://www.emro.who.int/pandemic-epidemic-diseases/ne ws/cholera-cases-decline-in-iraq.html.
UNICEF, Successful and Timely Efforts against Killer Disease Are Sustained in, 2016 [EN/AR] - Iraq | ReliefWeb [Internet]. 2016 [cited 2022 Jul 2]. Available from: https://reliefweb.int/report/iraq/successful-and-timely-efforts-against-kill er-disease-are-sustained-2016-enar.
OCHA, Cluster P. Inter-Cluster Analysis of Achievements and Gaps in Implementation of the 2022 HRP | HCT Meeting 5 July 2022 - Iraq | ReliefWeb [Internet]. 2022 [cited 2022 Jul 3]. Available from: https://reliefweb.int/report/
Educational campaigns to raise awareness of cholera in Baqubah]. Arabic [Internet [cited 2022 Jul 3]. Available from: https://moh.gov.iq/?page=4139, 2022.
health centers in Anbar Governorate intensify their campaigns on the dangers of epidemic diarrhea/cholera and hemorrhagic fever]. Arabi [Internet [cited 2022 Jul 3]. Available from: https://moh.gov.iq/?page=4161, 2022.
S. White, T. Heath, W. Khalid Ibrahim, D. Ihsan, K. Blanchet, V. Curtis, et al., How is hygiene behaviour affected by conflict and displacement? A qualitative case study in Northern Iraq, Mar 3 [cited 2022 Jul 2], in: H. Tappis (Ed.), PLoS One [Internet] 17, 2022, e0264434, 3, https://dx.plos.org/10.1371/journal.pon e.0264434. Available from.
S. White, A.H. Thorseth, R. Dreibelbis, V. Curtis, The determinants of handwashing behaviour in domestic settings: an integrative systematic review, International Journal of Hygiene and Environmental Health 227 (2020), 113512. Elsevier GmbH.
Euvichol-Plus®, ‘the world’s first plastic vial oral cholera vaccine,’ ready for global use – IVI [Internet] [cited 2022 Jul 4]. Available from: https://www.ivi.int/news -and-stories/press-releases/?mod=document&uid=956.
P.G. Ilboudo, M.A. Mengel, B.D. Gessner, B. Ngwira, P. Cavailler, J.B. Le Gargasson, Cost-effectiveness of a Reactive Oral Cholera Immunization Campaign Using ShancholTM in Malawi, Cost Eff Resour Alloc [Internet], 2021 Dec 1 [cited 2022 Jul 4];19(1):17. Available from: https://resource-allocation.biomedcentral. com/articles/10.1186/s12962-021-00270-y.
Shanchol | WHO - Prequalification of Medical Products (IVDs, Medicines, Vaccines and Immunization Devices, Vector Control) [Internet]. [cited 2022 Jul 4]. Available from: https://extranet.who.int/pqweb/content/shanchol.
S. Kanungo, A.S. Azman, T. Ramamurthy, J. Deen, S. Dutta, Cholera [Internet] The Lancet, 399, Elsevier B.V., 2022 [cited 2022 Jul 2]. p. 1429–40. Available from: htt ps://pubmed.ncbi.nlm.nih.gov/35397865/.
2022 Jul 14]. Available from: https://medicalguidelines.msf.org/en/viewport/ CHOL/english/management-of-a-cholera-epidemic-23444438.html.
Rehydration Therapy | Treatment | Cholera | CDC [Internet]. [cited 2022 Jul 4]. Available from: https://www.cdc.gov/cholera/treatment/rehydration-therapy.ht ml
J. Kühn, F. Finger, E. Bertuzzo, S. Borgeaud, M. Gatto, A. Rinaldo, et al., Glucosebut not rice-based oral rehydration therapy enhances the production of virulence determinants in the human pathogen Vibrio cholerae. Small PLC [cited 2022 Jul 4], in: PLoS Negl Trop Dis [Internet], 8, 2014 Dec 4, p. e3347, 12, https://dx.plos. org/10.1371/journal.pntd.0003347. Available from
Antibiotic Treatment | Treatment | Cholera | CDC [Internet]. [cited 2022 Jul 13]. Available from: https://www.cdc.gov/cholera/treatment/antibiotic-treatment. html.us
liefWeb. Cholera outbreak in Iraq: province/district laboratory-confirmed cases, 14 August - 30 December. ReliefWeb; 2024 [cited 2024 Aug 17]. Available from: https://reliefweb.int/map/iraq/cholera-outbreak-iraq-provincedistrict-laboratory-confirmed-cases-14-august-30-december
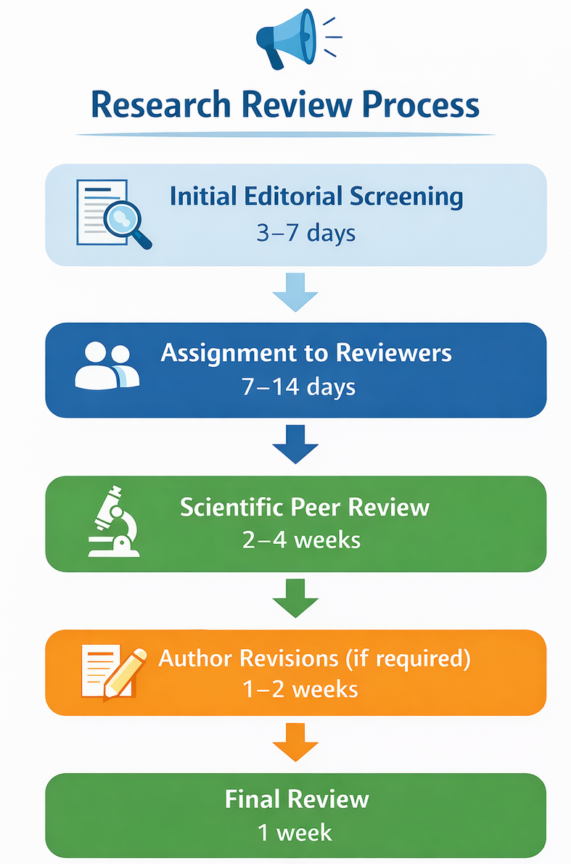
![Figure 2: Iraq: Province/district with laboratory-confirmed cases of cholera, August 14, 2007–December 30, 2007[81].](https://aijvm.aipublishers.org/public/journals/1/submission_35_35_coverImage_en.jpg)
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Academic International Journal of Veterinary Medicine

This work is licensed under a Creative Commons Attribution 4.0 International License.